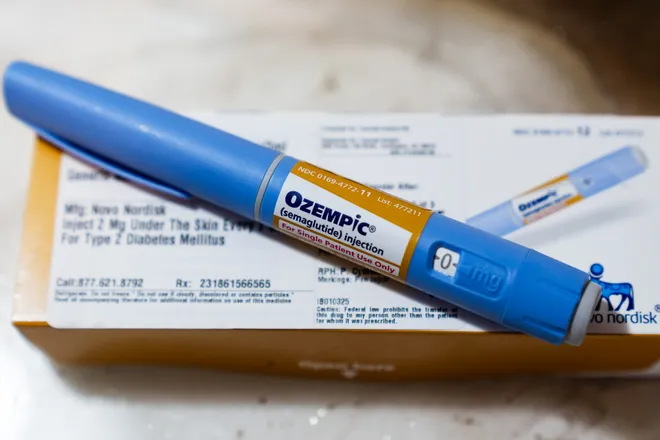
Why does Ozempic cost so much? Senators grilled Novo Nordisk CEO for answers.
Senators grilled the top executive of Novo Nordisk over why the Danish company charges Americans far more for the blockbuster weight-loss drug Wegovy and diabetes drug Ozempic than it does patients in Europe.
Novo Nordisk CEO Lars Fruergaard Jørgensen appeared before the Senate Committee on Health, Education, Labor and Pensions. The committee is chaired by Sen. Bernie Sanders, a Vermont independent who launched an investigation this year into Novo Nordisk's drug pricing.
Novo Nordisk has made nearly $50 billion on the sales of Ozempic and Wegovy since 2018, Sanders said. He described the U.S. as a "cash cow" for Novo Nordisk, accounting for 72% of the company's worldwide sales of those two drugs.
Among questions posed by Sanders: Why do Americans pay far more for these medications than patients in other countries?
Sanders opened the hearing by displaying charts comparing Novo Nordisk's prices charged to Americans and Europeans. The company charges U.S. residents $969 a month for Ozempic, but the same drug costs $155 in Canada, $122 in Denmark, and $59 in Germany.
For the weight-loss drug Wegovy, Americans pay $1,349 a month. The drug can be purchased for $186 in Denmark, $140 in Germany, and $92 in the United Kingdom, according to Sanders' charts.
"Nobody here is asking Novo Nordisk to provide charity to the American people," Sanders said. "All we are saying, Mr. Jørgensen, is treat the American people the same way that you treat people all over the world. Stop ripping us off."
Jørgensen defended the company's pricing of the wildly popular medications and said 80% of Americans can get these drugs for $25 or less per month.
He said U.S. list prices can't be compared to prices charged in other countries, in part, due to the nation's complex structure. U.S. prices are influenced by health insurance companies and drug-pricing middlemen called pharmacy benefit managers.
Jørgensen said the diabetes drug Ozempic is covered by the vast majority of private health insurance plans, as well as Medicare and Medicaid, the government health insurance programs for seniors and low-income families. Wegovy is covered by about half of private health insurers, Medicaid plans in 20 states and the Department of Veterans Affairs.
"You have said that our amazing medicines can't help patients if they can't afford them ‒ that is true," Jørgensen said. "It is also true that the full value of Ozempic and Wegovy can only be realized if patients can access them. Patients need affordability and access."
Medicare, the federal health program for adults 65 and older, is prohibited by law from covering drugs for those who are obese but otherwise do not have serious risk factors. But obese patients with diabetes or heart disease may qualify for coverage. The nonprofit health policy organization KFF estimated that 1 in 4 Medicare enrollees who are obese may be eligible for Wegovy to reduce their risk of heart attack or stroke.
The committee also highlighted a March study from researchers at Yale University found these drugs could be made for less than $5 a month, or $57 per year. Last week, Sanders announced CEOs of major generic pharmaceutical companies would be willing to sell Ozempic to Americans for less than $100 per month, at a profit. However, such estimates do not account for the expensive costs of researching and developing drugs and testing them in clinical trials.
Jørgensen said Novo Nordisk scientists have worked on the weight-loss drugs since the early 1990s. The company also has committed $30 billion to expand manufacturing capacity to address supply shortages of the medications.

Representatives of drug industry's trade group PhRMA said health insurers and pharmacy benefit managers deserve more scrutiny when it comes to drug affordability.
“The one question everyone should be asking is why aren’t insurers and PBMs being forced to answer for denying coverage and driving up patients’ costs?" said Alex Schriver, senior vice president of public affairs at PhRMA: "Senator Sanders continues repeating the same misleading rhetoric on drug prices. But why won’t he talk about how insurance conglomerates are taking in record profits or how PBMs are being investigated and sued for their abusive tactics?"
Disclaimer: The copyright of this article belongs to the original author. Reposting this article is solely for the purpose of information dissemination and does not constitute any investment advice. If there is any infringement, please contact us immediately. We will make corrections or deletions as necessary. Thank you.







